Getting Started in EMS
Updated October 27, 2025
Being an emergency healthcare provider is not as glamorous as Hollywood portrays, but it does provide the competent practitioner with a bit of local stardom and prestige, and occasionally a great deal of satisfaction.
In the US, healthcare licensing is regulated at the state level and the states are all different. Additionally, other US jurisdictions such as Puerto Rico and the military have their own regulations. So I am not going to pretend that I am an expert on continually changing EMS regulations, but I do have some observations, comments, and suggestions that will help the newbie.

Generally, to work as an emergency healthcare provider in the United States you must
- Be at least 18 years old,
- Have a high school diploma or GED certificate, and be physically capable of doing the work,
- Pass a background check,
- Successfully complete an EMS training course for the appropriate level of certification (which will be more clearly explained later.)
- Pass the National Registry of Emergency Medical Technicians (NREMT) exam for the appropriate level of certification,
- Get licensed by your state and pay for everything,
- Be certified by the medical director of the service that hires you,
- Be effective and stay out of trouble.
Age
Around the end of 2024, six states allow EMS workers to be younger than 18. Louisiana reportedly licensed a 15-year-old. The lad, however, was prevented from working due to the refusal of his service's insurance company to provide coverage.
Volunteer services typically require emergency healthcare providers to be 18 years old. Professional services typically require emergency healthcare providers to be 21 years old. An inter-facility transportation service might hire an 18-year-old as a junior crew member.
No state that I know of has an upper age limit. Maine's Bangor Daily News published an online article in 2015 about an 87-year-old woman who was working her last year as a volunteer EMT. The article did not say the size of the crew she was on, but I would assume it had at least two younger members. I would also assume that her organization was short of personnel and that her situation was highly unusual.
Prerequisites

The requirement to have an high school diploma or GED certificate is largely a requirement for state licensure, medical service certification, or insurability. The history of 15 and 16-year-olds in EMS is evidence that such an educational level in not carved in stone. In any case, one must be able to read, write, and do basic math. One must also be physically able to recognize and perform interventions, carry equipment, and move patients. Dropping a patient is never excusable.
There is a record of at least one legally-deaf man being an EMT, but that was many years ago. I do not think there is now any EMS service in this country that would hire a deaf person. A volunteer squad might take on a deaf person as a third rider, but emergency response requires good hearing, and there are other places in healthcare that a deaf person could work.
A Background Check

Passing a background check is a standard requirement for anyone providing patient care but may not be needed before enrolling in classes. (In Texas, students typically must spend some time working both in a hospital and on an ambulance as part of their education.)
Some services are willing to overlook some criminal convictions. If you have a record, do not try to hide it. If you are rejected as an EMT, there are other healthcare jobs that might be open to you. These include opportunities in long-term care facilities, home care agencies, group homes, and adult day care centers. Decisions depend on the circumstances of the offenses, supply and demand of healthcare workers, an individual's attitude, and state laws.
It should go without saying that one must also be legally permitted to work in the United States.
An EMS Training Course
Apparently, there is no lower or upper age limit to enrolling in and completing an EMS training course, but some educators have their own age-restrictive policies. Some school districts offer EMS classes as part of a high school curriculum. The NREMT has no lower or upper age limit for certification, but there will likely be a limit between the time of EMS course completion and eligibility for NREMT certification.
I imagine that most states require Federal Emergency Management Administration (FEMA) certification in the National Incident Management System (NIMS) and the Incident Command System (ICS). The exact courses required depend on the level of EMS certification being pursued. Many of these courses are free. See my ICS Overview page for a common English description of the subject.
Some states require OSHA hazardous materials training at an awareness level, and I assume that all requiire professional-level CPR training from an organization such as the American Heart Association or the American Red Cross.
Texas requires a Texas jurisdiction training certificate. The course for it is mind numbing.
Online Training
Some states allow the book-learning to be completed online at the EMR and EMT levels. Some testing and practical skills are taught in-person. I did this for both my EMR and EMT training. There are a couple advantages and several disadvantages to this.
The primary advantage is that it allows you to work on your own schedule. In theory, you could complete the course in several weeks; take up to a year to complete the course; or study for several weeks, take a couple months off, and then finish-up. The other advantage is that if you live in a rural area, it could be your only practical option.
The primary disadvantage is that it takes a huge amount of self-discipline and initiative. In my case, the book-learning was fairly straightforward, although I did have to purchase a hard copy of the text. Trying to read a pdf of 1400 page book on a PC screen was intolerable. Another disadvantage is that learning the practical skills on my own was difficult. I am surprised I passed the tests. It helps if you have someone to practice with.
Personal interaction with others, including an experienced instructor, is an important part of learning. Hearing EMS war stories from others helps create the mindset needed to prepare for the stress of the job. This was more greatly appreciated when I met my in-person "boot-camp" instructors who included two flight paramedics, one of whom had been an army ranger. The story of a burn patient who was too contorted to be airlifted is one that has stayed with me.
While doing my hospital rotations, I crossed paths with a professional advanced EMT who got his start with the same online school that I attended, but while doing my ambulance rotations, my supervisor expressed that he had a low opinion for online training.
NREMT Certification

The National Registry of Emergency Medical Technicians is a non-profit agency responsible of overseeing the education of pre-hospital medical providers by standardized testing and certification. Sometimes called the National Registry, it now recognizes four levels of certification, which from the lowest to highest are:
- Emergency Medical Responder (EMR),
- Emergency Medical Technician (EMT),
- Advanced Emergency Medical Technician (AEMT),
- Paramedic.
You will likely see other provider designations in states and services. For example, according to Texas law, a person trained at the EMR level is called an Emergency Care Attendant (ECA). In some services (judging from old jackets and patches) you might see an EMT-A (EMR), an EMT-B (EMT), an EMT-C (AEMT), EMT-P (Paramedic,) or a multitude of other designations.
As of early 2025, four states, New York, Wyoming, Illinois, and North Carolina, do not recognize NREMT testing or certification as a prerequisite for licensure. This is not to imply that they have lower standard, just that they have their own systems.
One advantage of the National Registry is that it facilitates reciprocity, meaning that, where allowed by state law, a licensed emergency healthcare provider in one state may work in another state without requiring to be licensed in the other state. This is especially useful for transferring patients between states either by air or ground.
The National Registry uses "emergency healthcare provider" as a collective descriptor for its various levels of certification. Thus, it would be logical to use the abbreviation EHP as well, but this has yet to catch on.
Getting your State License
If Wikipedia is to be believed, state licensure is all over the map. Hawaii and Florida have only two levels: EMT and Paramedic. New Jersey has three levels. Pennsylvania has ten levels, which includes Medical Command Physician (MCP). Montana recognizes four levels and five endorsements. Ohio, home of the NREMT, is one of the few states that follow the four NREMT levels of licensure.
Texas is another interesting case. In Texas there are five levels of licensure, and the state's law gives a great deal of leeway at the local level concerning the level of care a provider is allowed to perform. Thus, an ECA (EMR) in west Texas could work at the level of an EMT in Houston.
Around 2018 there was a provision in Texas law that allows non-licensed workers to crew an ambulance under certain circumstances. I do not know the last time this was used or if it still an option, but I suppose it is intended to provide coverage in sparsely populated areas. The thought must have been that somebody with limited EMS training is better than nobody.
Another Texas nuance is that Texas licensure is commonly referred to as certification in the law but is occasionally referred to as licensure on official websites. (More about nomenclature later.)
The cost for a Texas state certification (or licensure) varies by level a few other factors but is typically less a couple hundred dollars. Other fees might that might not be covered by the basic EMS class tuition include a book, a stethoscope, fingerprinting, and NREMT membership fees.
Medical Director Certification
This is one of the most critical parts of EMT regulation to know for staying out of legal trouble.
Emergency healthcare providers practice medicine under the license of a medical doctor (i.e. the medical director.) They may not do deviate from what their medical director allows. Anything beyond what is permitted is called "freelancing," and is considered to be practicing medicine without a license which is a crime that can lead to prison time.
Emergency healthcare providers are allowed to practice basic first aid while off duty but not medicine. The difference between the two is nuanced and beyond the scope of this article, but it is something that you need to know.
Record Keeping
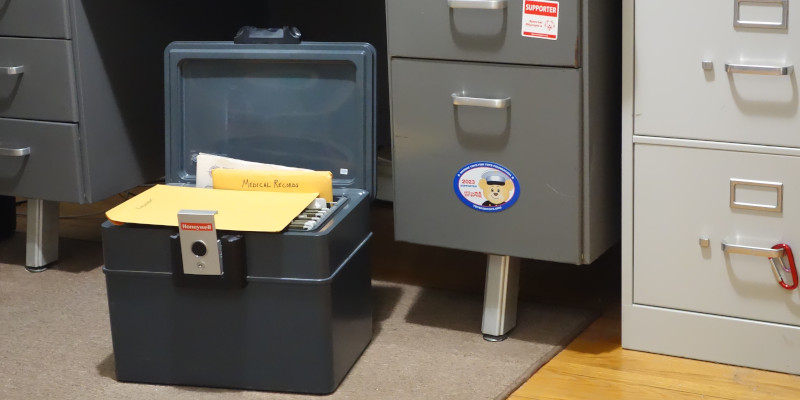
If you served in the military, you will likely know what a me-folder is. It is a large manilla envelope in which a service person keeps his or her personal records. I strongly recommend a new emergency healthcare provider adopt this approach. I have three: one for medical records, one for EMT paperwork, and one for employment. I keep them in a fire-protective box along with insurance, home, automotive and tax records. I also have many of my records scanned and backed-up on a flash-drive that I store off-site.
Nomenclature and Protocols
From the earliest days of your EMS journey, you will likely be confronted with the fact that medicine often has multiple words for the same thing or procedure.
There are numerous reasons for this that would take way too much space to elucidate. Just be aware that you will have to know redundant vocabulary, so it will not throw you off balance. I found it very annoying at first but am now (largely) used to it.
A similar point can be made about protocols, which takes us back to medical direction and staying out of trouble. Protocols are extremely important rules about what to do or not do in particular situations. They vary from service to service and are all over the map.
The good news about protocols is that once you get hired, you will only need to concentrate on your local ones.
Specialization
I do not know much about this subject, but there is other training that emergency healthcare providers can take to expand their opportunities. This includes training for work as ski patrollers, flight paramedics, critical care paramedics, community care paramedics, tactical paramedics, wilderness paramedics, and dive medics. Experience with emergency medical response is also an important skill to have for emergency dispatchers. See the National Organizations section on my Links Page.

I find flight medicine to be especially interesting. I have been told that there are two levels of certification in Texas: fixed wing and rotary wing. As I understand it, much of the training involves learning how changes in air pressure affect patient care. Because flying is involved, the FAA has a hand in regulation. I suppose insurance companies are also involved. And I suppose that the state department is involved when patients are transferred across international borders.
Before you get too excited about flying around providing healthcare, know that about half of the names in the Texas EMS Hall of Honor arrived by air.
Pay
Volunteers obviously do not get paid, which is a big problem in some rural services because basic paramedic training typically lasts two years. But even for professionals, pay is nowhere commensurate to the value of service provided. Again, this is simply a function of the supply and demand of emergency healthcare providers.
EMS is a relatively easy and inexpensive way into the medical profession, and many see street EMS as a "tour of duty" that helps them transition into another healthcare roll such as a physician, nurse, or physician assistant. A seldom-mentioned benefit of certification is that EMT will look good on any résumé and will help you stand out if you search for a career outside of healthcare.
In some areas of the country and in some specialties, the pay can be good, but do not expect it alone to make you rich or to provide an upper-middle class level of living.
Continuing Education
I suppose all states require continuing education to maintain licensure. The EHP has the responsibility to keep up on this and not wait until the last moment. Many have had their licenses suspended for not completing this on time and then lying about it.
Honey Trapping and other Temptations
Occasionally I will read of an EMS service getting sued because of allegations of sexually inappropriate behavior by an emergency healthcare provider, and my first thought is "honey trap."
Honey trapping is an investigative or exploitative practice involving the use of romantic or sexual relationships for interpersonal, political, or monetary gain. It is one of the more painful ways to get into trouble and can be instigated by a patient looking for a payout.
In Texas, sexually inappropriate behavior is behavior that exploits the EMS personnel-patient relationship in a sexual way.... and is non-diagnostic and/or non-therapeutic, may be verbal or physical, and may include expressions or gestures that have sexual connotation or that a reasonable person would construe as such.
While honey trapping is one of the more reported-on failures in EMS, other pitfalls include poor record keeping, poor driving, failing to report physical or emotional abuse of a patient by anyone, dishonesty on any level, and even any activity that betrays the public trust and confidence in EMS.
One More Requirement
This subject applies to all levels of emergency healthcare providers, but I will use an EMT as an example.
Getting trained, certified, licensed, and hired will not make you a real EMT. Becoming a real EMT takes experience. Typically, it will be about a year and a half in a busy 911 service before your peers consider you to be a brother or sister.
So stay open to learning; stay focused; stay respectful, polite, and humble. If you get a big head, it will get knocked off.

